Introduction: Understanding Pelvic Floor Dysfunction
Pelvic Floor Dysfunction (PFD) is a common yet often overlooked condition that affects millions of people worldwide—both men and women. Despite its prevalence, many individuals live with symptoms for years without a proper diagnosis, often mistaking them for normal aging or unrelated health issues.
The pelvic floor plays a crucial role in bladder control, bowel function, sexual health, and core stability. When these muscles do not function correctly, it can significantly impact quality of life. This article explores pelvic floor dysfunction symptoms, causes, diagnosis, and modern treatment options, helping patients and caregivers make informed decisions.
What Is Pelvic Floor Dysfunction?


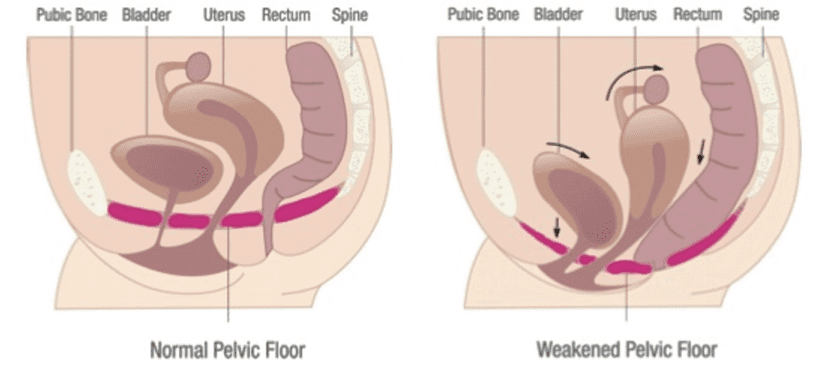
Pelvic Floor Dysfunction occurs when the muscles and connective tissues that support the pelvic organs (bladder, uterus/prostate, and rectum) become too weak, too tight, or poorly coordinated.
Normally, pelvic floor muscles contract and relax to:
- Control urination and bowel movements
- Support pelvic organs
- Enable sexual function
- Stabilize the spine and core
When this coordination fails, everyday functions can become painful or difficult.
Common Symptoms of Pelvic Floor Dysfunction
Symptoms vary depending on muscle weakness, tightness, or nerve involvement. Many patients experience more than one symptom at the same time.
Urinary Symptoms
- Frequent urination
- Urinary urgency or leakage
- Difficulty starting urine flow
- Incomplete bladder emptying
Bowel Symptoms
- Chronic constipation
- Straining during bowel movements
- Fecal incontinence
- Feeling of incomplete evacuation
Pelvic Pain & Discomfort
- Pelvic pressure or heaviness
- Pain during intercourse (dyspareunia)
- Tailbone or lower back pain
- Rectal pain or spasms
Sexual Health Issues
- Erectile dysfunction in men
- Painful penetration in women
- Reduced sexual sensation
According to Cleveland Clinic, pelvic floor dysfunction often goes undiagnosed because symptoms overlap with gastrointestinal and urinary disorders.
What Causes Pelvic Floor Dysfunction?
Pelvic floor dysfunction rarely has a single cause. Instead, it develops due to a combination of physical, neurological, and lifestyle factors.
1. Pregnancy and Childbirth
- Vaginal delivery
- Prolonged labor
- Use of forceps or vacuum extraction
2. Aging and Hormonal Changes
- Muscle weakening with age
- Reduced estrogen levels after menopause
3. Chronic Strain
- Long-term constipation
- Heavy lifting
- Chronic coughing
4. Pelvic Surgery or Trauma
- Hysterectomy
- Prostate surgery
- Pelvic fractures
5. Neurological Conditions
- Stroke
- Multiple sclerosis
- Spinal cord injury
The National Institute of Diabetes and Digestive and Kidney Diseases highlights chronic straining as a leading but preventable cause.
Types of Pelvic Floor Dysfunction
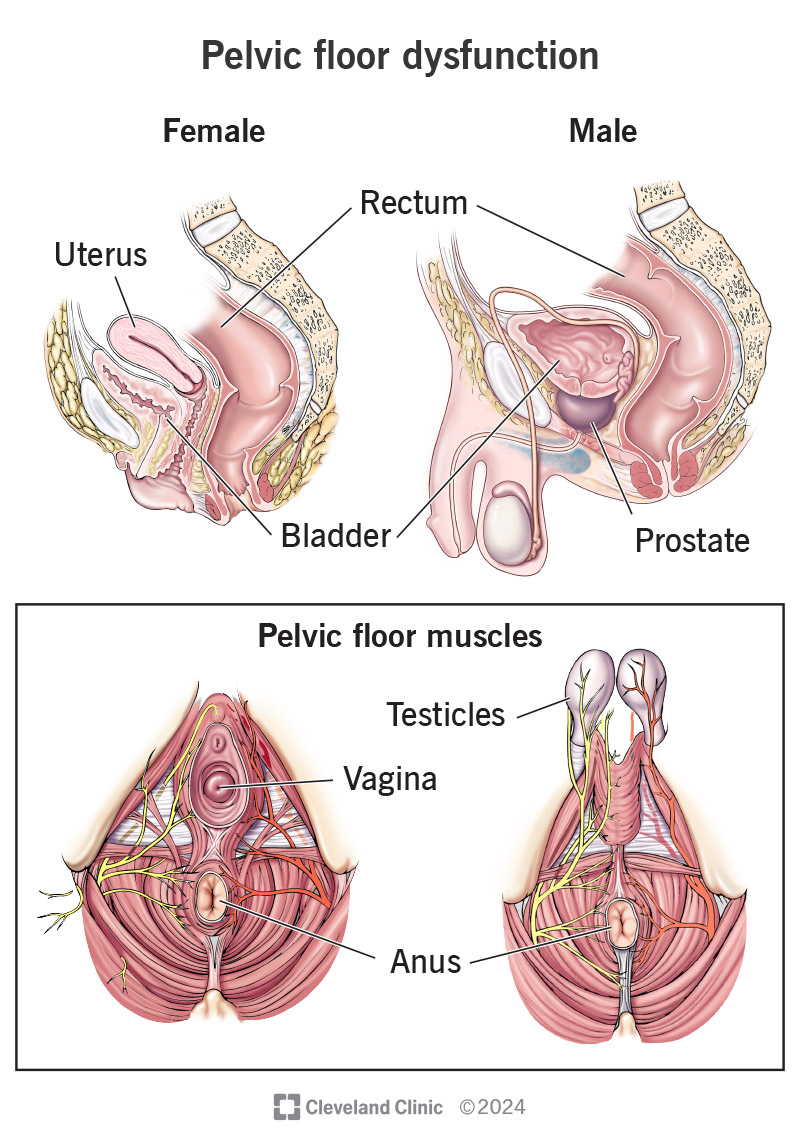
Understanding the type of dysfunction helps guide treatment.
Hypotonic (Weak Pelvic Floor)
- Stress urinary incontinence
- Pelvic organ prolapse
Hypertonic (Overactive or Tight Pelvic Floor)
- Pain during urination or intercourse
- Difficulty relaxing muscles to empty bladder or bowels
Incoordination
- Muscles fail to relax during bowel movements
- Often seen in chronic constipation
How Is Pelvic Floor Dysfunction Diagnosed?
Diagnosis is typically non-invasive and tailored to symptoms.
Diagnostic Methods Include:
- Detailed medical history
- Physical pelvic examination
- Pelvic floor muscle assessment
- Ultrasound or MRI imaging
- Urodynamic testing
Healthcare providers often follow guidelines from the American Urological Association when evaluating bladder-related symptoms.
Treatment Options for Pelvic Floor Dysfunction
Treatment focuses on restoring muscle balance, not just strengthening.
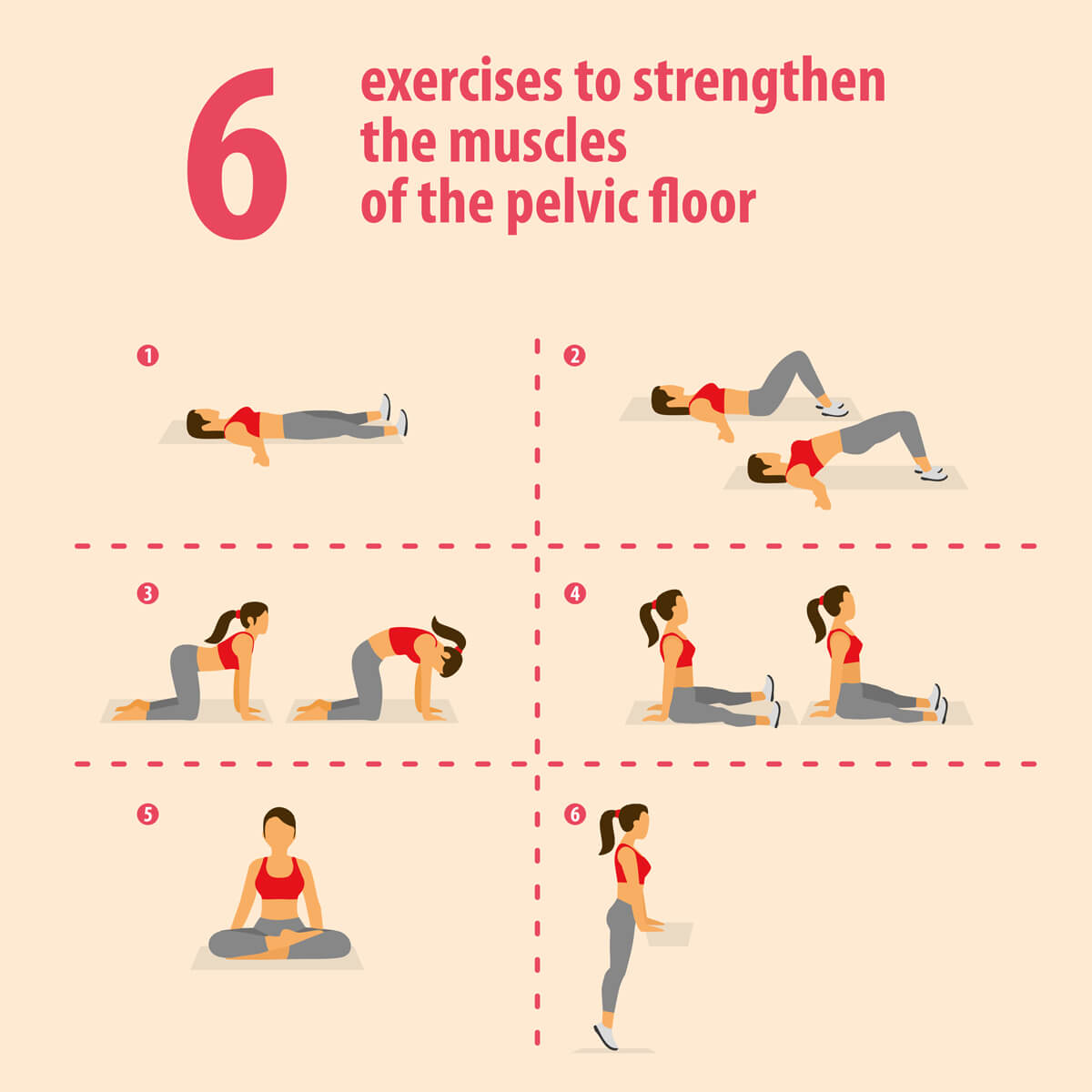
1. Pelvic Floor Physical Therapy (First-Line Treatment)
- Manual muscle release
- Guided relaxation techniques
- Functional strengthening exercises
This is considered the gold standard for most patients.
2. Biofeedback Therapy
- Sensors measure muscle activity
- Helps patients learn proper muscle control
3. Lifestyle & Behavioral Changes
- Proper toileting posture
- Dietary fiber optimization
- Avoiding chronic straining
4. Medications
- Muscle relaxants (for hypertonic muscles)
- Stool softeners
- Pain management medications
5. Advanced Treatments (Severe Cases)
- Botox injections for muscle spasm
- Neuromodulation therapy
- Surgical correction (rare and selective)
According to Mayo Clinic, most patients improve significantly with conservative therapy alone.
Can Pelvic Floor Dysfunction Be Prevented?
While not all cases are preventable, risk can be reduced by:
- Treating constipation early
- Practicing correct lifting techniques
- Avoiding excessive Kegels without guidance
- Seeking postpartum pelvic care
When to See a Specialist
You should consult a pelvic health specialist if you experience:
- Persistent pelvic pain
- Ongoing urinary or bowel control issues
- Painful intercourse
- Symptoms lasting more than a few weeks
Early intervention leads to faster recovery and prevents long-term complications.
Final Thoughts
Pelvic Floor Dysfunction is treatable, manageable, and more common than most people realize. The key is awareness, proper diagnosis, and individualized care. Ignoring symptoms can lead to worsening discomfort, while early treatment often restores normal function and quality of life.
If you or someone you care for is experiencing symptoms, seeking help from a trained pelvic health professional can be life-changing.





